Full Thickness Macular Holes
A Full Thickness Macular Hole (FTMH) is a hole in the retina that occurs in the central part of the macula (known as the fovea).
FTMHs are relatively common – about 3 in every 1000 persons over the age of 55 develop a macular hole.
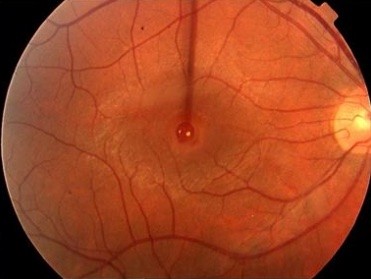
Full Thickness Macular Hole
Most people develop this problem in their 60’s and 70’s and women are affected more commonly than men. The risk of both eyes developing a full thickness macular hole is approximately 10-15%.
Repair of a FTMH requires an operation.
Causes
Most Full Thickness Macular Holes develop without an obvious cause.
Rarely, a FTMH develops after a severe eye injury or retinal detachment.
FTMH develop because of an abnormal interaction between the vitreous and the retina.
The vitreous fills the central part of the eye, and is normally in contact with the retinal surface. In patients with macular holes, this vitreo-retinal contact is abnormally strong, causing the vitreous to exert traction on the retinal surface. This ultimately causes the fovea to split and a ‘full thickness macular hole’ forms. Sometimes very fine scar tissue occurs on the retinal surface (an epiretinal membrane), which also contributes to traction on the macular hole.
In the early stages of FTMH development, spontaneous resolution can occur. But once a completed defect in the retina forms, spontaneous resolution is rare and FTMH tend to enlarge as time passes.
Symptoms.
Visual loss, particularly difficulty reading, and distorted vision are the most common symptoms in patients with full thickness macular holes. Vision loss may come on rapidly but sometimes it is only noticed when the good eye is covered. Vision typically stabilizes at a poor level, and the side or peripheral vision is usually retained.
Examination
A thorough eye examination is required to diagnose a FTMH.
Vision is tested, both for distance and near tasks. The pupils are dilated to allow careful inspection of the vitreous and retina. The macula is evaluated and it is also important to thoroughly examine the peripheral retina. Commonly, you will be asked to look at a narrow vertical line of light. When a FTMH is present, this line becomes very thin or even breaks in two at its central point (Watzke-Allen test).
Investigation
The diagnosis of a FTMH is confirmed by retinal photography and OCT imaging. The OCT gives a detailed anatomical picture of the FTMH, recording its size and important relationships such as vitreous traction on the edges of the hole or the presence of an epiretinal membrane.

OCT of FTMH showing vitreous traction on the edge of the macular hole
Management of Full Thickness Macular Holes
Surgery is the only way of treating FTMHs and improving vision.
Surgery is possible in almost every patient with a macular hole.
Surgery is performed in hospital, usually under assisted local anaesthetic, which is safe, extremely effective and which allows for rapid postoperative recovery.
The surgical operation used to treat full thickness macular holes is a specialized microsurgical procedure called a vitrectomy.
Small instruments are passed into the centre of the eye . An instrument called a ‘vitreous cutter’ cuts and aspirates the vitreous and carefully separates the vitreous from the retinal surface and the edge of the macular hole. Then the surface layer of the retina (the internal limiting membrane) around the macular hole is removed, typically with the assistance of a special blue dye called Brilliant Peel©.
Once the vitreous and any surface retinal membranes have been removed, the eye is filled with a gas called sulfur-hexafluoride (SF6). This gas is used to push on the retina at the site of the hole, holding the edges of the hole together while the eye works to seal the macular hole.
After surgery, face down positioning is required.
Face down positioning is an important part of the treatment of FTMHs. It places the macular hole at the ‘top’ of the eye, and allows the gas, (which naturally rises to the top of the eye) to hold the hole closed whilst healing takes place. Face down positioning should be maintained during both the day and the night, at all times except when eating, washing or going to the toilet.
The duration of face down positioning is currently 3 – 5 days, but there is a trend to even shorter periods of strict positioning for most patients.
Tips for face down posturing
- Change position between lying directly face down on the bed (with pillows arranged to allow breathing), and sitting up and leaning forward with the forehead resting on a pillow on a table.
- At night, face down posturing is difficult. Sleep with the face turned slightly to one side.
- Hire a ‘posture chair’, which most people find useful
(Click here to read up on vitrectomy recover chair and bed support) - Don’t posture whilst eating meals, washing or going to the toilet. Posture at all other times.
The gas is slowly reabsorbed by the eye, taking about 2 weeks to disappear completely.
Flying is not permitted until the gas is completely reabsorbed.
Eye drops are required for the first 3-4 weeks after surgery.
Outcome of Surgery
Vitrectomy leads to closure of macular holes in 80 – 90% of cases. These days, the success rate is almost 95%.
When the FTMH closes, 70 – 80% of patients gain an improvement in vision of more than 2 lines (on the vision chart). Visual acuity of 6/12 or better was achieved by 58% of patients in one North American study. Visual results are better when the hole has been present for only a short period of time, and when the macular hole is smaller.
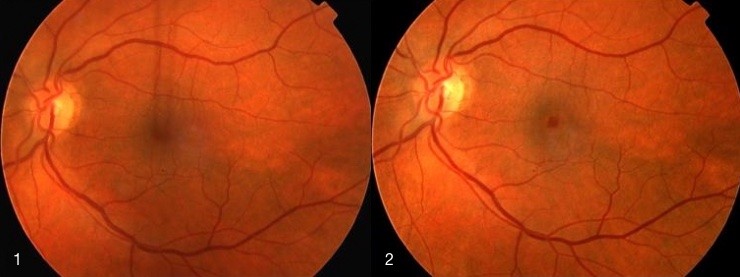
1. Macular hole before surgery. Vision 6/60, 2. Macular hole after surgery. Vision 6/9
Deciding to have Vitrectomy Surgery for a Full Thickness Macular Hole
Most patients with a FTMH should have surgery to repair the hole, since vision deteriorates if the hole is not treated, and because surgery is safe and has a high rate of success. It offers the only way of stabilising and improving visual acuity, which occasionally improves almost to normal.
There are, however, some important considerations before deciding upon surgery.
- Post-operative face-down posturing for is arduous but achievable. Special arrangements might need to be made by those patients who live alone.
- The vitrectomy procedure is safe, having the same overall level of risk as a cataract operation. The most important side effects and risks are:
a.Cataract formation: Most patients require cataract surgery within 1 year.
b.Retinal detachment develops in 1-2% of patients after surgery. An operation is needed to fix the retinal detachment.
c.A loss of some of the peripheral field of vision is found in up to 14% of patients, although many are not aware of this loss until they are formally tested.
d.Other risks include bleeding, infection, inflammation, and elevated intraocular pressure (glaucoma). The risk of complete loss of vision in the operated eye is 1/1000, which is equivalent to the risk of a cataract operation.
This information is a guide. If you have a specific question, please ask Dr Downie or Dr Simunovic.
