Age-related Macular Degeneration
Age-related macular degeneration (AMD) is the most common cause of vision loss in our community.
It causes degeneration of the central part of the retina, which is known as the macula. The macula is responsible for clear, detailed colour vision, and is the part of the retina used when reading, driving, and looking at faces and TV.
In patients with AMD, central vision is affected, but modern treatments are effective at minimising vision loss.
Who is affected?
Macular degeneration usually affects people over the age of 50 and becomes more common with increasing age. About 1 in every 10 Australians over the age of 50 have MD and up to 30% of people more than 80 are affected.
What are the symptoms and how does the disease progress?
AMD progresses slowly, over many years. There is a long period before symptoms develop when changes are visible in the macula. Vision is affected only late in the course of the disease.
The first symptoms reflect wearing out of the macula (known as “dry” macular denegeration) and may include the slow onset of difficulty reading, some mild distortion, and slow adaptation to dim conditions – such as coming inside to a dark room after being in strong sunlight. If wearing out progresses, central vision can be affected.
The most worrying change is the sudden onset of decreased vision, a blur or dim patch in the central vision and distorted vision.
If there is an abrupt (over days) change in vision with any of these symptoms, it is vital that you see your ophthalmologist as soon as possible.

Distortion and loss of central vision (scotoma)
These symptoms usually mean that an abnormal blood vessel (known as a choroidal neovascular membrane or ‘CNVM’) has formed under the retina. This is commonly called “wet” macular denegeration. Wet macular degeneration only develops in a minority of patients with AMD, but causes the greatest amount of vision loss. Effective treatment to stabilise and even improve vision is available, but the best results are achieved when treatment is begun as soon as possible
What happens to the eye?
Macular degeneration develops because the supportive layer under the retina, the RPE, degenerates. It is akin to the underlay under your carpet wearing out, so that the carpet itself is affected. Degeneration is due to the accumulation of waste products from the retina in the RPE, disrupting its function.
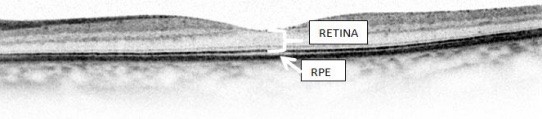
Normal OCT showing RPE
The main early change is the appearance of drusen (white deposits of debris under the retina) and some clumps of pigment. Gradually the RPE and the retina (the ‘underlay and the carpet’) wear out (this is called ‘atrophy’).
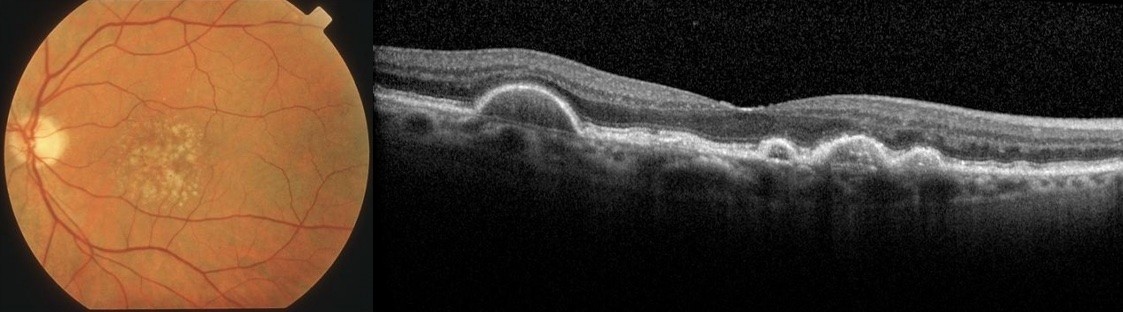
Drusen
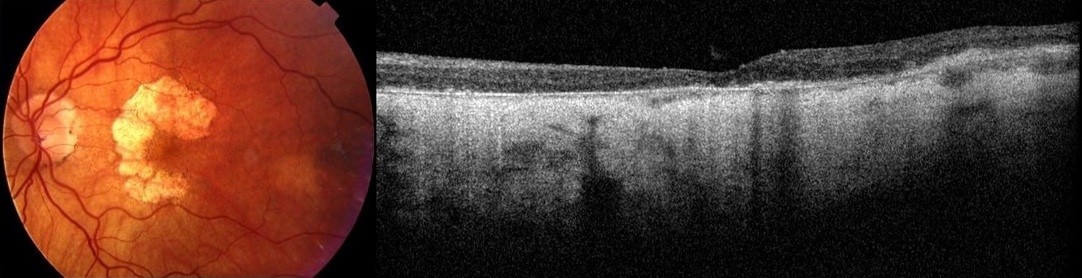
Atrophic change around the central macula
In some people, the damaged RPE lets an abnormal blood vessel grow under the retina (a CNVM). This is called wet ARM because the abnormal vessel leaks fluid and blood. Untreated, it leads to scar formation that destroys the central part of the macula, causing severe visual loss.
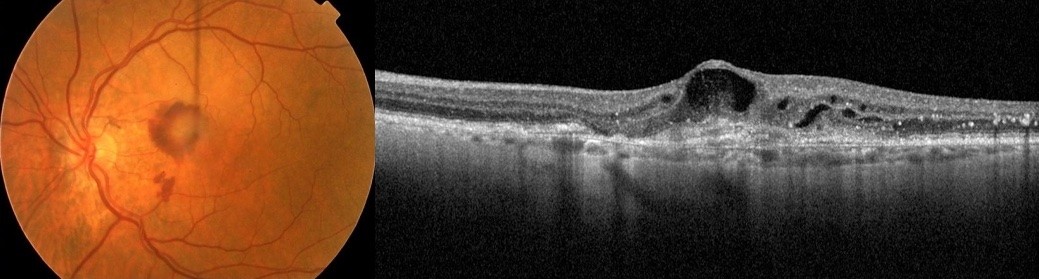
Choroidal Neovascular Membrane (CNVM or Wet MD)
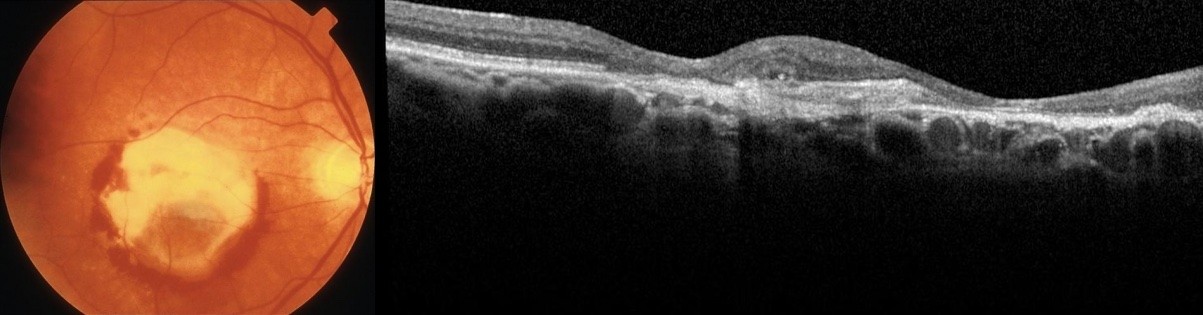
Disciform scar which has destroyed central vision
Investigations undertaken to confirm the presence of a CNVM include OCT imaging and Fluorescein Angiography.
Can I prevent macular degeneration?
While there are no specific treatments for early AMD, there are some important measures that can be taken to minimise the risk of developing AMD and, perhaps, slow its progression.
The risk factors for developing AMD include age, family history, dietary factors and smoking.
If a close relative is affected, or you are a smoker, you are four times more likely to develop AMD than someone who does not have these risk factors.
To reduce your risk of developing AMD and to slow the progress of the disease:
- Don’t smoke.
- Eat a diet rich in vegetables, fruits, fish and low in both vegetable and animal fats. Even one fish meal per week has been shown to decrease the risk of vision loss by half in some studies.
- Wear a hat and sunglasses when outside.
- Have your eyes regularly examined by an ophthalmologist ( a medically trained eye doctor).
- If examination of the retina shows changes of early AMD (i.e. drusen are present):The use of high dose antioxidant vitamins has been shown to decrease the risk of vision loss and to slow the progression of the disease.
There are a number of preparations available, but all include a combination of Vitamins C and E and zinc. Some include additional antioxidants such as Lutein and zeaxanthin and fish oil, although the benefit of these additional products hasn’t yet been proven. - Check your vision at home regularly. Check the vision in each eye separately, to check for the development of wet ARM.The use of a simple grid (known as an amsler grid) helps in this test: look for the onset of blurred vision, a central dark patch or central distortion.
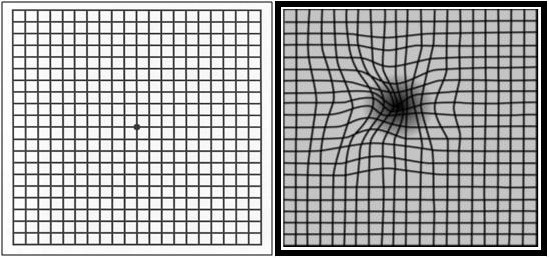
Amsler Grid test: left is normal; right indicates central blurring and distortion which often indicates the development of WET Macular Degeneration (a choroidal neovascular membrane).
If there is a sudden change in the central vision in one eye, with blurring, a central dark patch or central distortion of the lines on the amsler grid, then you need to be reviewed by your ophthalmologist urgently.
What treatments are available for Wet AMD?
Treatment of CNVM (choroidal neovascular membrane), or wet Macular Degeneration , is very effective.
A long course of injections of Lucentis, Eylea or Avastin directly into the eye is effective at controlling the growth of the abnormal blood vessel. These medicines are antibodies that block the action of chemicals within the eye that cause abnormal blood vessels to grow.
Vision stabilises in most patients and improves significantly in about one third of people who are treated. A major determinant of final vision is the amount of damage done to the macula by the abnormal blood vessel, which is why early detection of the CNVM is so important.
Assessment and ongoing management of patients with CNVM is very specialised. The doctors at Retina & Eye Consultants uses the most advanced imaging to detect and monitor wet AMD, and our staff are highly trained and experienced in the care of patients with this problem, with the aim of maximising the vision of our patients with ARM and minimising the risks of treatment.
