Diabetic Eye Disease
Diabetes is increasingly common in Australia, with more than 8% of people affected.
Diabetes changes involve many parts of the body, including the eye. The most important effect of diabetes on the eye is on blood vessels in the retina, which is known as “diabetic retinopathy".
Diabetic retinopathy is the most important cause of blindness in working age Australians.
What can you do to prevent diabetes affecting your eyes and vision loss?
There are effective ways of slowing the development and progression of diabetic retinopathy, and of treating its complications, to prevent blindness.
These are:
- Maintain good control of blood sugar levels, and other risk factors such as raised blood pressure and cholesterol. This is very effective at delaying the onset and progression of diabetic retinopathy.
- Have regular eye checks looking for diabetic retinopathy.
This is vital and should start as soon as diabetes is diagnosed. Your family doctor will refer you for a check with your ophthalmologist. Try to organise the check with your ophthalmologist at the same time each year, so that it’s easier to remember.
Regular checks allow for early detection of diabetic retinopathy and for timely treatment. Treatment for diabetic retinopathy is less effective at improving or stabilising vision if presentation is delayed and severe changes are present. - Effective treatment, which can stabilise and even improve vision, is available for sight threatening complications of diabetic retinopathy. This requires expert care – the ophthalmologists in our practice are highly skilled in delivering these treatments. Laser therapy to the retina is still the mainstay of treatment, but new modalities of treatment including injection of medications into the eye, and surgery, are available to help preserve and improve vision.
What happens when diabetes effects the retina?
Diabetic retinopathy is caused by damage to the retinal capillaries. They become leaky or block off, or both.
Characteristic changes include microaneurysms, small haemorrhages and ‘cotton wool spots’ (which are small areas where the retinal capillaries are blocked off, causing a lack of blood supply or “ischaemia”). These changes generally don’t effect vision and constitute ‘Non-proliferative diabetic retinopathy’ (NPDR). However, if these abnormalities progress, vision can fall.
There are two important changes in the retina that can cause vision loss:
1. Clinically Significant Macular Oedema (CSMO). Excessive leakiness from capillaries in the central part of the macula causes the retina to swell and malfunction. Retinal swelling that is near to, or involves, the central macular area is called ‘clinically significant’. This is the most common cause of vision loss in diabetics.
2. Proliferative Diabetic Retinopathy (PDR). If too many of the retinal capillaries block off, the accumulated damage to the retina (called ischaemia) leads to the growth of abnormal blood vessels on the retinal surface: ‘proliferative retinopathy’. These abnormal vessels can bleed (causing vitreous haemorrhage) and scar tissue associated with the abnormal vessels can pull on the retina and cause it to detach. PDR is less common than CSMO but it can lead to severe vision loss and blindness if not appropriately treated.

1.Non-Proliferative Diabetic Retinopathy, 2. Proliferative Diabetic Retinopathy
How is diabetic eye disease managed?
The monitoring, management and treatment of diabetic retinopathy is a complex and specialised part of ophthalmic practice. Assessment of diabetic retinopathy includes a detailed examination of your whole eye and your retina, which is supplemented by advanced imaging techniques including fundus photography, OCT imaging that measures the thickness of the retina, and fluorescein angiography that demonstrates the retinal circulation. These examinations and investigations guide treatment. It is also important that the results of your eye assessments and treatments are communicated to your family doctor and diabetes specialist, since general factors such as your blood sugar control, high blood pressure, blood count and kidney disease can affect the severity and stability of diabetic retinopathy.
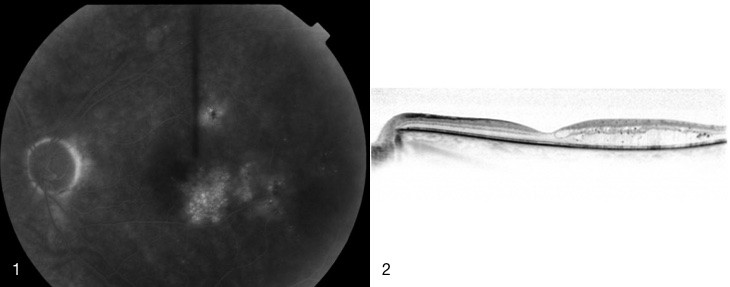
1. Fluorescein angiogram of CSMO, 2. OCT showing retinal swelling due to CSMO
What treatments are available?
The treatment of diabetic retinopathy is complex. The important components of treatment are:
- Optimising diabetic control and the control of other systemic factors such as high blood pressure. For example, good control of blood sugar levels can decrease the rate of development of diabetic retinopathy by 75%, and the progression of established retinopathy by 50%.
- Retinal laser treatment is the mainstay of treatment for the eye.
- Supplementary treatments are being increasingly employed to manage severe diabetic retinopathy. These include the use of medicines that are injected directly into the eye, and also microincisional vitrectomy surgery.
Treatment for CSMO
Treatment for CSMO usually begins with light laser to the area of swollen retina in the macula. This treatment is safe and painless. It decreases the chance of visual loss but generally doesn’t lead to improvement in vision. It may need to be repeated.
If CSMO is severe and involves the centre of the macula, there is accumulating evidence that treatment with injections of medicines into the eye, such as Avastin, Triamcinolone (a steroid) and Lucentis, are more effective than laser alone in improving and stabilising vision.
Treatment for PDR
Treatment for PDR requires urgent retinal laser, sometimes also supplemented by intraocular injections and by surgery. Laser for PDR differs from that used in CSMO. The aim of laser is to create multiple scars in the peripheral area of the retina. This stops the release of ‘growth factors’ that make the abnormal blood vessels grow – so that they wither away. Laser is extensive and generally needs to be applied over a number of visits.
It is heavy and somewhat uncomfortable. Usually there are no long term side effects, but sometimes vision can fall during treatment and not return to its previous levels. We do everything possible to minimise the discomfort and side effects of laser for PDR, but it’s always important to remember that the consequence of inadequate treatment of PDR is blindness.
If there are severe complications such as vitreous haemorrhage or traction retinal detachment associated with PDR, vitrectomy surgery may be needed.
Diabetic Retinopathy is one of the most important retinal conditions that we treat at retina consultants. We frequently develop a long term relationship with diabetic patients and their other medical carers, which is very satisfying. We are also involved in research projects aiming to improve the care of all patients with diabetic retinopathy.
