Epiretinal Membrane
It is also known as ‘premacularfibrosis’, ‘cellophane maculopathy’ or ‘macular pucker’.
An epiretinal membrane is a thin layer of transparent scar tissue on the surface of the retina in the macula.
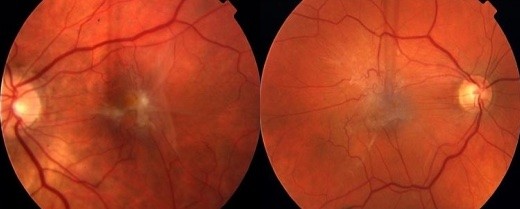
Images of the Epiretinal Membrane
How common are epiretinal membranes?
An epiretinal membrane occurs commonly with ageing. Approximately 7% of people over the age of 50 years have some degree of epiretinal membrane formation, and it becomes more common with increasing age. Up to 15% of people over the age of 85 years have an epiretinal membrane.
What are the symptoms of epiretinal membrane?
Most epiretinal membranes cause few symptoms and don’t require treatment.
However, in some patients the membrane thickens and begins to contract, resulting in wrinkling and thickening of the underlying retina. This affects vision, often with the following symptoms:
- Blurred vision
- Distorted vision: straight lines (eg. doorways, venetian blinds and telephone poles) appear wavy
- These symptoms can disrupt binocular vision
- Progression is often slow, but can occasionally be rapid and pronounced
What are the causes of epiretinal membrane?
Most epiretinal membranes occur without an obvious cause. A posterior vitreous detachment is usually present, which seems to permit the development of an epiretinal membrane in some people.
Less often, an epiretinal membrane can be secondary to other eye conditions such as:
- Retinal tears and detachment
- Inflammation within the eye
- Retinal blood vessel disorders (eg retinal vein occlusion)
- Diabetic retinopathy
- Severe trauma
How is an Epiretinal Membrane diagnosed?
An epiretinal membrane is diagnosed by examining and imaging the retina.
Your vision is tested, and you will be asked to look at an amsler grid to document the presence of distortion. Then, your pupils are dilated to allow examination of the retina, which is undertaken at the slit lamp by the doctor.
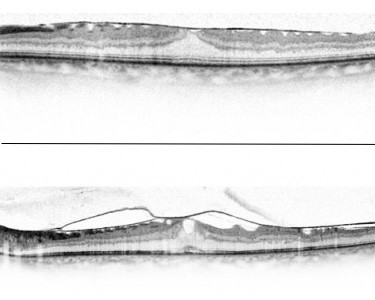
An OCT of an epiretinal membrane
The presence of an epiretinal membrane is documented with retinal photographs and a special test called an OCT (Optical Coherence Tomography). This instrument is able to give a microscopic view of the retinal structure.It records the anatomy of the retina including its thickness and the degree of wrinkling due to the epiretinal membrane. Only occasionally is a further test called a ‘fluorescein angiogram’ required.
What is the treatment of an epiretinal membrane?
An epiretinal membrane is treated with surgery. Modalities including drops and laser are not effective and do not improve vision.
Therefore, the important decision is whether or not surgery is required.
Many epiretinal membranes cause no symptoms and can be observed.
However, surgery is indicated when symptoms are sufficiently severe. This is an individual decision, but the usual indications for surgery are:
- Poor vision
- Distorted vision in one eye that interferes with overall vision
- Severe anatomical or structural changes in the retina
- Progression of symptoms and structural changes, which will ultimately be associated with poor vision. In this setting, it is best to intervene before damage becomes permanent.
Vitrectomy surgery for epiretinal membrane.
An epiretinal membrane is treated by surgery.
Surgery is performed in hospital, usually under assisted local anaesthetic, which is safe and comfortable.
The surgical procedure is a specialised microsurgical operation called a vitrectomy. The surgeon performs modern sutureless microincisional vitrectomy surgery, which allows for more effective surgery and more rapid and comfortable recovery.
During the vitrectomy procedure very fine instruments are placed into the eye, through small holes in the sclera. The vitreous gel is removed and the epiretinal membrane is then grasped and ‘peeled’ from the retinal surface. Typically, a special dye called Brilliant Peel© is used intraoperatively to increase the visibility of the epiretinal membrane
At the end of the operation, the eye is filled with a large bubble of air, which is spontaneously reabsorbed over 5-7 days.
Special posturing after surgery is not usually required, apart from a need to sleep on one side or the other at night whilst air is inside the eye.
Most patients require 1-2 weeks off work, and use eye drops for 3-4 weeks post operative.
The results of vitrectomy surgery for epiretinal membrane.
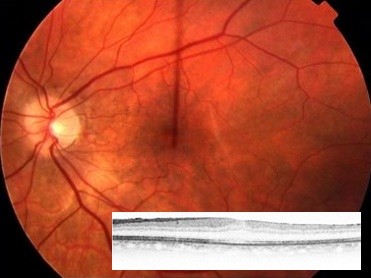
After vitrectomy and removal of the epiretinal membrane. Inset: OCT after removal of the epiretinal membrane
Vitrectomy surgery for epiretinal membrane is a safe and effective procedure.
It takes a number of months for the macula to smooth out and recover after an epiretinal membrane is removed, so vision is usually not its best for 3-4 months.
Vision improves in the majority of patients, but usually doesn’t return to be completely normal. Distortion is generally reduced and this can be the most gratifying benefit of surgery.
Approximately 80% of patients gain an improvement in vision of 2 lines or more on the vision chart. In other patients, vision stabilises and ongoing deterioration is prevented, even if visual acuity doesn’t improve.
Vitrectomy surgery always brings on a cataract (an opacity in the lens of the eye), and it is important to remember that vision after surgery for an epiretinal membrane is often not its best until this cataract has been removed.
Apart from this, complications of surgery are uncommon. The vitrectomy procedure is safe, having the same overall risk as a cataract operation. The most important side effects and risks are:
- Retinal tear form during the operation in 5-7% of cases. These are treated at the time of surgery, and don’t have a long-term effect on vision.
- Retinal Detachment develops in 1-2% of patients after surgery. An operation is required to treat this problem.
- Other risks include bleeding, infection, inflammation, and elevated intraocular pressure (glaucoma).
- Inflammation in the fellow eye is very rare (1/10 000).
- The risk of complete loss of vision in the operated eye is very uncommon (about 1/1000, which is equivalent to the risk of a cataract operation).
Deciding to have vitrectomy surgery for an epiretinal membrane.
Vitrectomy for an epiretinal membrane is a specialised but safe and effective procedure. Surgery is indicated if visual symptoms are interfering with your daily activities and particularly if changes associated with the epiretinal membrane are progressing.
Please feel free to discuss this decision, and any other questions, with Dr Downie or Dr Simunovic.
